
A historic agreement to offer obesity medications like Wegovy, Zepbound, and Mounjaro at an unprecedented $149 per month, an 88.6% decrease from the current $1,000–$1,350 list price, is being finalized by the Trump administration.
Medicare coverage for eligible beneficiaries under a novel “Most Favored Nation” policy would be part of this agreement, which could be announced as early as November 5, 2025. In order to compel pharmaceutical companies Eli Lilly and Novo Nordisk to accept significant discounts in return for tariff relief, this initiative uses trade tariffs. In an effort to combat the country’s obesity epidemic and significantly reduce out-of-pocket expenses, the Centers for Medicare & Medicaid Services (CMS) is also testing a program to cap obesity medication costs for Medicare beneficiaries.
Pharmaceutical Price Negotiations’ Historical Background

Due to the federal government’s limited ability to negotiate, drug prices in the United States have historically remained high. Prior to recent legislative changes, direct price negotiations were prohibited for Medicare, the largest payer. By using trade tariffs, a tactic typically employed against foreign rivals, as a weapon to force Big Pharma to cut costs, the Trump administration’s push to negotiate prices under the “Most Favored Nation” clause represents an uncommon change in policy.
This approach stands in stark contrast to earlier administrations that either tolerated increases in pharmaceutical prices or relied on softer pricing pressures. The price reduction for obesity medications is currently the biggest single-drug reduction, demonstrating the federal government’s unprecedented ability to influence healthcare costs.
The Market Demand and the Obesity Epidemic

There is a huge need for efficient treatments because 138 million Americans, or 42% of the country’s adult population, are obese. GLP-1 receptor agonist medications, such as Wegovy and Mounjaro, have gained widespread popularity despite their high current costs because of their demonstrated effectiveness in clinical trials demonstrating an average weight loss of 15%.
If cost barriers are removed, there is enormous potential for widespread adoption. Medicare’s affordable access could significantly increase the number of users beyond adults with private insurance, particularly older Americans who face significant health risks from obesity. By acknowledging obesity as a chronic, treatable condition rather than a lifestyle choice, this agreement has the potential to spark a paradigm shift in healthcare.
The $149 Price’s Pharmacoeconomics

Financial barriers would be significantly reduced if obesity medication costs were reduced to $149 per month, which would result in an annual savings of $10,200 to $12,600 per patient when compared to current pricing. Ten million Americans would save almost $120 billion a year if they had access to these medications at the new rate.
The savings could significantly reduce healthcare costs for both individuals and the government, especially in light of Medicare’s potential expansion to cover up to 20 million obese beneficiaries. Drug manufacturers may, however, accept lower revenue per unit in exchange for higher volume sales and tariff relief, indicating a strategic shift away from niche high-margin profits and toward mass-market accessibility.
Leadership Dynamics and Political U-Turns
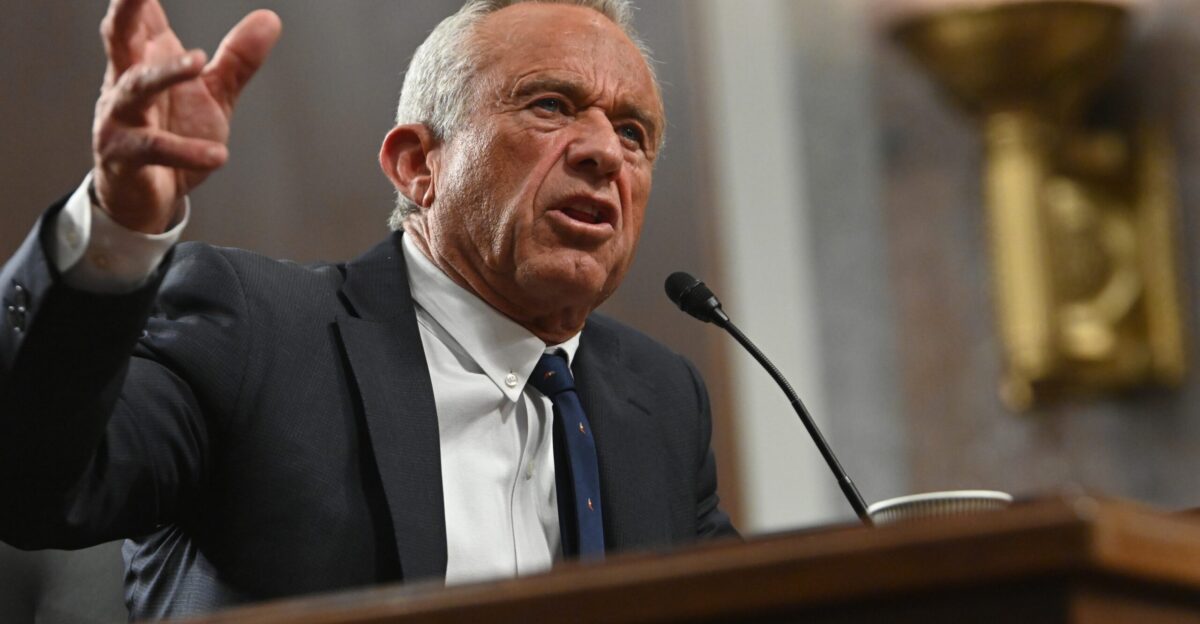
After joining the administration, Robert F. Kennedy Jr., the Health Secretary, changed his public stance against obesity medications, once referring to Americans as “stupid and addicted”, to support more widespread drug access. The pragmatic changes occurring within federal policymaking are highlighted by this six-month ideological reversal.
The Biden administration’s stalled, more cautious Medicare drug expansion plans contrast with the Trump administration’s pressure tactics, exhibiting an aggressive, trade-leverage strategy that surpasses conventional political approaches. A volatile but potentially revolutionary period in U.S. healthcare governance is indicated by these shifting alliances and the evolution of internal policies.
Medicare Coverage Pilot and Possible Repercussions

CMS is expanding Medicare’s disease-treatment portfolio by launching a pilot program to cap out-of-pocket costs for certain Medicare beneficiaries obtaining obesity medications. If expanded, this could be the largest increase in Medicare-covered chronic illness treatments since the Part D prescription drug benefit was introduced in 2006.
However, early access may be restricted by initial program restrictions, such as eligibility requirements or pre-authorization requirements, which could lead to discussion about equity and long-term affordability. The careful balancing act between limiting federal spending and addressing a public health emergency for millions of obese seniors is reflected in this pilot.
Tariffs to Reduce Prices

Pharmaceutical companies exchange lower prices for relief from punitive tariffs that target imported goods or components as part of the administration’s innovative quid pro quo negotiations.
This is the first time in American history that trade policy has been used to control domestic healthcare costs. Tariffs are now a blunt tool to fight monopolistic pharmaceutical pricing, a sector infamously resistant to regulation, even though they have historically targeted trade deficits and foreign competition. In addition to undermining pharmaceutical companies’ pricing power, this tactic combines healthcare and economic policy in ways that may have an impact on future drug pricing negotiations across the industry.
Benefits to Public Health and Patient Outcomes

According to clinical data, GLP-1 medications reduce body weight by an average of 15%, or about 33 pounds for a person who weighs 220 pounds. Tens of millions of people could lower the country’s obesity-related morbidity if these treatments were widely used at a monthly cost of $149. Beyond medication costs, this weight loss may lead to fewer cases of diabetes, a lower risk of cardiovascular disease, and a decrease in healthcare utilization.
Effective pharmacological treatment of obesity may reduce the burden of secondary chronic illnesses, increase worker productivity, and lower long-term healthcare costs. Public health could undergo unprecedented change as a result of the ripple effects.
Implications for Pharma Revenue and Market Changes

In exchange for tariff relief and increased market penetration, Eli Lilly and Novo Nordisk will probably lose over $10 billion in high-margin U.S. obesity drug revenue each year, marking a strategic turning point. This change indicates a shift away from exclusive pricing power and toward volume-based tactics more akin to consumer goods than specialty pharmaceuticals.
A shift like this could push cost-efficiency improvements, realign R&D priorities, and signal a more commercialized pharmaceutical industry for obesity treatments. Widespread adoption could stabilize overall revenues and build resilience against public backlash on pricing, even as earnings per patient sharply decline.
Is $149 a Trojan Horse or a Sustainable Price?

Opponents caution that the $149/month price may solidify a lifetime reliance on expensive medications with ambiguous long-term safety profiles. The medicalization of body weight raises ethical concerns because pharmaceutical companies may be able to maintain profits through perpetual renewals rather than cures.
Furthermore, pre-authorization requirements and restrictions mentioned during Medicare enrollment may dampen enthusiasm and restrict access to better-off or motivated patients. The “deal” could be a Trojan horse, increasing the role of pharmaceuticals in the treatment of chronic illnesses while neglecting lifestyle and preventative measures. Policymakers are challenged by this paradox to strike a balance between sustainable health paradigms and accessibility.
Comparing Pharmaceutical Pricing Structures Worldwide

In the past, the United States has spent up to ten times as much on drugs as other developed nations. Arguments that higher R&D costs necessitate higher U.S. prices are undermined by this deal’s $149 monthly rate, which places obesity medications closer to international price standards.
The administration challenges the global pricing structure of the pharmaceutical industry through trade leverage. This might spark international pricing ripple effects or even promote multilateral pharmaceutical price negotiations, which could lead to more extensive reexaminations of pharmaceutical valuation and pricing across other chronic conditions.
Psychological and Socioeconomic Aspects

By portraying obesity as a chronic illness that is treatable and supported by the federal government, accessible obesity medications could lessen the stigma attached to the condition. By confirming that obesity is more than just a personal issue, this change may enhance mental health outcomes. Socioeconomic disparities still exist, though, as lower-income groups frequently have higher rates of obesity but encounter obstacles when trying to access healthcare.
Vulnerable groups may be disproportionately burdened by navigating Medicare programs and drug approvals even with price reductions, highlighting the need for outreach and education to stop growing health disparities. The agreement also calls into question the narratives of empowerment versus pharmaceutical dependency in public health messaging.
Future Directions and Unexplored Policy Hypotheses

Such pricing agreements may be the first step toward a universal drug pricing framework that incorporates volume-based reimbursements and real-world outcomes, according to emerging theories. This could encourage businesses to focus on population health effects rather than just sales volume.
Furthermore, the tariff-for-price model might serve as a model for other costly drug categories, such as treatments for Alzheimer’s or rare diseases, which could change the health economics of the United States. In order to avoid tariff-triggered agreements, pharmaceutical companies may decide to withdraw medications or restrict national supply, which could present regulatory challenges. Agile oversight frameworks must be anticipated and designed by policymakers.
Dissecting the Significance of RFK Jr

Political pragmatism triumphing over ideology is demonstrated by Robert F. Kennedy Jr.’s shift from outright anti-pharma rhetoric to endorsing mass obesity drug accessibility. His previous derogatory comments, which referred to Americans as “stupid and addicted” to drugs like Ozempic, stand in sharp contrast to his current position on policy.
This points to a larger trend in which administration priorities and public health emergencies can significantly alter people’s positions. It also alludes to the strategic compromises and intense, behind-the-scenes pressures that characterize contemporary healthcare governance. His metamorphosis serves as an example of how political narrative framing affects public acceptance of pharmaceutical interventions and drug policy discourse.
A Revolution in the Management of Obesity and Drug Costs

The impending $149 monthly obesity medication deal represents a disruptive turning point in American healthcare: a significant price reduction attained through unconventional trade pressure, signifying a change in the financing and provision of pharmacotherapy for chronic illnesses. The agreement raises concerns about sustainability, equity, and industry strategy even though it promises significant cost savings and increased access for millions.
It may spark more extensive changes by upending long-held beliefs about the treatment of obesity and pharmaceutical pricing structures. Transparent implementation, strong Medicare integration, and striking a balance between innovation incentives and public health imperatives, a difficult but essential evolution in addressing America’s obesity crisis, are essential for success.