
The U.S. is in its most intense flu season in nearly three decades. During the week ending December 27, flu-like illness made up 8.2% of all outpatient visits—the highest share since national tracking began in 1997. Roughly one in ten people who saw a doctor had flu symptoms.
By late December, at least 11 million Americans had been infected, hospitalizations topped 120,000, and deaths reached 5,000, with the peak still ahead.
Slide 2 – A Season That Broke the Record Books

This surge is not a routine winter wave. The 8.2% visit rate marks the first time in 29 years that flu-like illness crossed the 8% threshold nationwide.
Forty-eight states are reporting elevated flu activity, with 45 classified as high or very high, including Alabama, Colorado, Georgia, Minnesota, and New York, and an additional 3 experiencing moderate but still significant spread, including South Dakota and West Virginia, leaving only a handful with low or minimal levels. Health officials describe the map as “predominantly red,” signaling near-total national saturation at a point when the season typically has not yet peaked.
Why This Flu Is Different

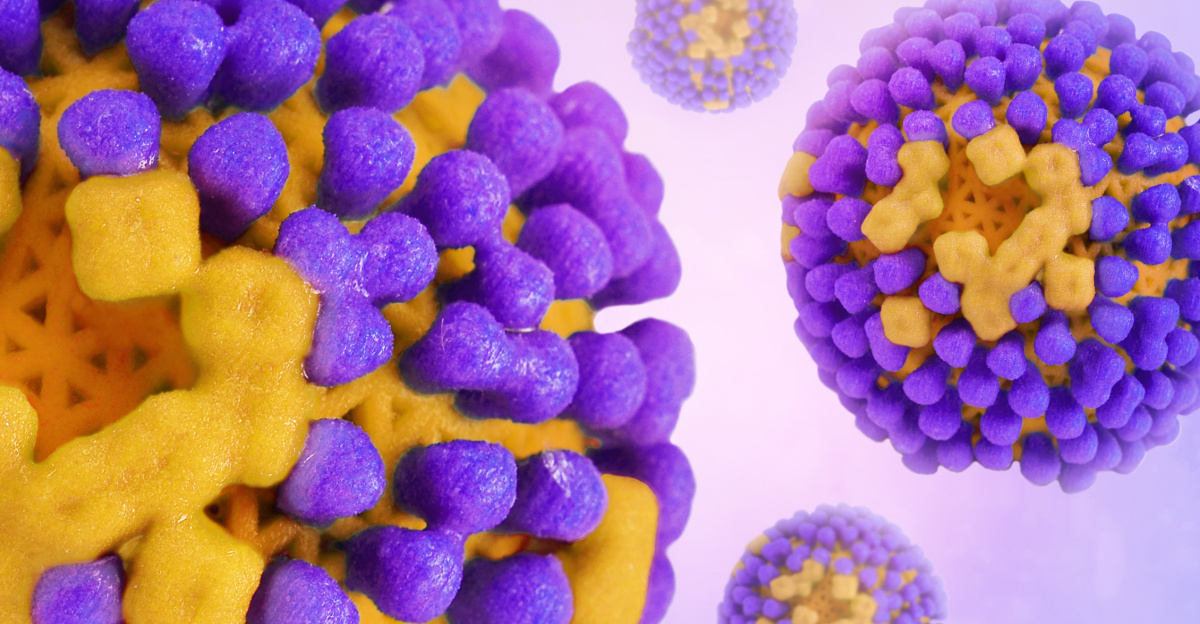
The dominant driver is influenza A(H3N2) subclade K, a fast-spreading variant that emerged after vaccine strain decisions were finalized. More than 90% of subtyped cases are H3N2, and most of those belong to subclade K.
The variant carries ten mutations on its hemagglutinin surface protein, helping explain its rapid global spread and why this season escalated earlier and faster than usual.
Vaccine Mismatch, Uneven Protection

Vaccination still helps, but protection varies by age. Early assessments show the vaccine is about 72–75% effective in children and teens against subclade K, but only 32–39% effective in adults.
Overall vaccination coverage remains low: about 42% of adults and children were vaccinated by mid-December. That leaves tens of millions exposed, especially seniors, who tend to suffer more severe illness from H3N2 strains.
Hospitals Under Immediate Strain

Hospitalizations are climbing sharply. During the week ending December 27, more than 33,000 patients were admitted nationwide for flu. The weekly hospitalization rate rose to 8.4 per 100,000 people, up from the week before.
Cumulatively, this season already ranks as the third-highest hospitalization rate at this point since 2010–11, stressing emergency departments, inpatient units, and staffing schedules across the country.
New York’s Alarming Milestones

New York State illustrates the pressure vividly. In just one week, 4,546 flu hospitalizations were reported—an all-time state record and a 24% increase from the prior week.
Case counts set records too, with more than 72,000 infections reported in a single week. State officials reported nearly 1,000 additional hospital admissions in just seven days, underscoring the rapid intensification of the surge.
Children in the Crosshairs

Young people account for a large share of care visits. About 35% of outpatient respiratory visits are among those under 24, and children under five make up roughly 20% of flu-like illness visits.
Pediatric risk looms especially large after last season’s grim benchmark: 289 pediatric flu deaths in 2024–25, the deadliest non-pandemic season on record, with most deaths among unvaccinated children.
Back-to-Back Severe Seasons

Consecutive severe seasons defy typical flu patterns, where bad years are often separated by milder ones. The current 2025–26 season follows directly after last year’s historic pediatric toll.
Epidemiologists note that immunity gaps from the pandemic era, early seasonal timing, and rapid viral evolution may be combining to produce unusually intense, consecutive outbreaks rather than isolated spikes.
Clinics, ERs, and Wait Times

As flu visits surge, routine care competes with urgent respiratory cases. Emergency rooms report longer waits, crowded triage areas, and increased use of temporary overflow spaces.
Outpatient clinics see schedules packed with fever and cough visits, pushing non-urgent appointments further out. The pressure ripples across healthcare, from diagnostic labs processing tests to pharmacies managing antiviral demand.
Healthcare Workers Feeling the Impact

The strain is not just about beds. Healthcare workers are also getting sick, shrinking available staffing during peak demand. Hospitals must juggle overtime, reassignments, and delayed leave.
In some regions, infection-control rules require unvaccinated staff to mask during patient care, adding operational complexity while leaders warn the system must brace for several more difficult weeks.
Schools and Families Disrupted

Rising absenteeism has forced temporary school closures and attendance drops in multiple states. Some districts report a quarter or more of students out sick, along with significant staff absences. For families, closures trigger childcare scrambles and missed workdays.
For children who rely on school meals or services, even short disruptions can carry outsized consequences.
Economic Ripples Begin to Form
Flu seasons already cost the U.S. tens of billions of dollars in lost productivity and medical care. With hospitalizations rising early and fast, costs are expected to climb higher this year.
Employers face absenteeism, healthcare systems absorb staffing expenses, and insurers see growing claims. The economic impact builds quietly but steadily as the virus spreads through workplaces and communities.
A Global Pattern Emerges

What the U.S. is experiencing mirrors trends seen abroad. Subclade K circulated widely in the Southern Hemisphere earlier in 2025, where some countries logged record flu activity.
As the variant spread across continents, it established itself quickly, signaling that this is not a localized anomaly but part of a broader global influenza pattern.
Behavior Shifts at Home

As awareness grows, households adjust. Demand rises for fever reducers, thermometers, and air humidifiers. Many people limit gatherings, work remotely when possible, or mask in crowded indoor spaces.
Telehealth visits for flu symptoms climb as patients seek faster access to care without waiting rooms, subtly reshaping how people interact with the healthcare system during peak weeks.
The Shadow of Pediatric Loss

Last season’s pediatric death toll hangs over the current surge. Health officials repeatedly emphasize that most children who died previously were not fully vaccinated.
That statistic has sharpened messaging around childhood vaccination and early treatment. For many families, the numbers transform influenza from a familiar nuisance into a deeply personal and urgent threat.
Treatment Windows Matter

Antiviral medications can reduce severity, but timing is critical. Doctors stress that treatment works best when started within 48 hours of symptom onset.
Delays—whether from crowded clinics or uncertainty about symptoms—can mean missed opportunities to blunt illness. Clear guidance urges people to seek care promptly rather than waiting for symptoms to worsen.
Why the Peak Still Lies Ahead

Flu activity typically crests in January or February, and experts caution that current data likely precedes the high point. Holiday travel and gatherings from late December may not yet be fully reflected in case counts.
With widespread transmission already established, models suggest continued increases over the next several weeks before any sustained decline.
What Individuals Can Do Now

Health guidance remains straightforward: get vaccinated if you have not, even now; seek care quickly for symptoms; isolate when sick; and protect vulnerable family members.
Masking in crowded indoor settings and staying home when ill can slow spread. These steps do not eliminate risk, but collectively they reduce pressure on hospitals and communities.
A Test of Preparedness

This season is testing the resilience of healthcare systems and public trust. Record visit rates, uneven vaccine uptake, and rapid viral change expose weaknesses while highlighting the value of surveillance, communication, and early intervention.
The response over the coming weeks will shape not only this season’s outcome, but readiness for those ahead.
One Virus, Nationwide Consequences

The 2025–26 flu season shows how quickly a familiar pathogen can reshape daily life. Clinics overflow, schools pause, workplaces adapt, and families worry.
With millions infected and the peak still approaching, the lesson is stark: influenza remains a powerful force. Preparedness, vaccination, and timely care remain the most reliable tools as the country moves through the hardest stretch.
Sources:
“Weekly US Influenza Surveillance Report: Key Updates for Week 52, ending December 27, 2025.” Centers for Disease Control and Prevention, 7 Jan 2026.
“Flu-like illness activity now at highest rate on record, new CDC data shows.” ABC News, 4 Jan 2026.
“New York reports record-breaking number of flu hospitalizations in a single week.” ABC News, 1 Jan 2026.
“2024-2025 Pediatric Flu Deaths Surpass Previous Record.” Families Fighting Flu, 31 Dec 2025.